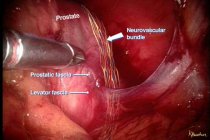
For patients with clinically localized prostate cancer, nerve-sparing robotic prostatectomy provides patients with a safe and minimally invasive technique for removal of the prostate gland, while preserving as much of the surrounding nerve structures responsible for penile erections.
For patients with clinically localized prostate cancer, nerve-sparing robotic prostatectomy provides patients with a safe and minimally invasive technique for removal of the prostate gland, while preserving as much of the surrounding nerve structures responsible for penile erections.
This minimally invasive approach has the advantage of smaller incisions, reduced pain, blood loss, transfusion rates and hospital stay, as compared to conventional open surgery with a similar cure rate. In select patients with locally invasive or metastatic cancer, morbid obesity, bleeding tendencies, or severe heart or lung problems, robotic prostatectomy may not be advised.
The Operation
Robotic prostatectomy requires that patient undergo a general anesthesia. While operative time varies from one individual to another, the average operating time is approximately 3-4 hours.
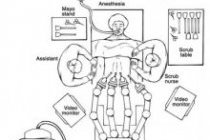
During robotic prostatectomy approximately 6 small keyhole (< 1cm) incisions are made in the abdomen (Figure 1), through which portals or trocars are placed to allow passage of instrumentation into the abdomen.
The abdomen is filled with carbon dioxide gas to create a larger working space for the surgeon to accomplish the operation. This gas is later evacuated from the abdomen at the conclusion of the operation. The surgeon controls 3 multi-jointed robotic instruments to accomplish the tasks of dissection, cauterization, cutting and suturing with the same dexterity as the human wrist (Figure 2).
In addition, the surgeon controls a stereoscopic lens connected to a high definition camera which provides a three dimensional, high definition view of the internal anatomy. A highly skilled surgical assistant stands at the operating table assisting the surgeon by exposing and retracting tissue using instrumentation inserted through two of the trocars.